Agentic AI,
Artificial Intelligence & Machine Learning,
Industry Specific
Concerns Over Preauthorization Denials Are Escalating
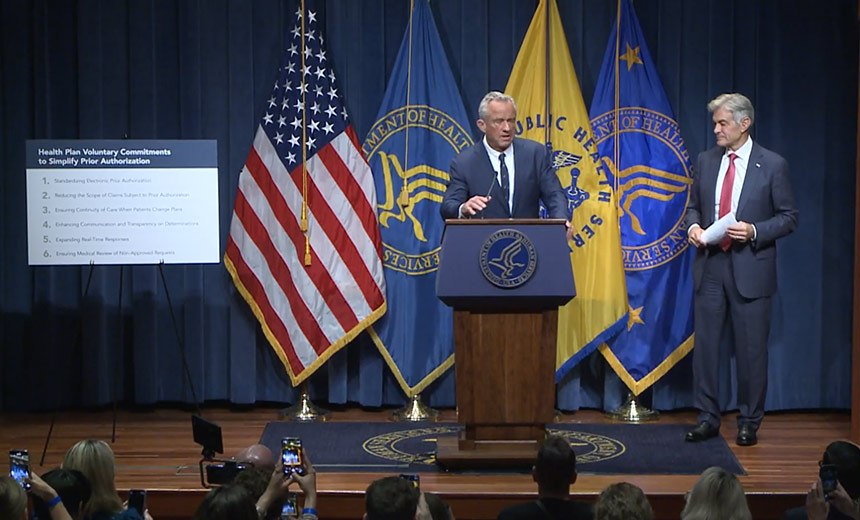
Recent developments have seen major health insurers, covering approximately 80% of Americans under Medicare, Medicaid, and commercial plans, collaborating with the U.S. Department of Health and Human Services (HHS) to enhance preauthorization processes. These changes follow increasing frustrations from healthcare professionals regarding the lengthy and often confusing procedures tied to preauthorization requests.
Historically, preauthorization has been a significant administrative burden for physicians and a key point of dissatisfaction. Insurers have faced criticism and even legal action for their reliance on artificial intelligence (AI) technologies that have led to the denial of crucial claims. HHS officials voiced concerns that such denials can jeopardize patient health outcomes, particularly for urgent procedures.
This initiative was announced following a roundtable discussion in Washington, D.C., with leaders from top insurance firms. Representatives from Aetna, Blue Cross Blue Shield Association, Centene Corp., Cigna Group, and others attended, with indications that more insurers will join the effort. The focus is on reducing dependence on antiquated methods such as faxes and complicated web portals that impede timely preauthorization.
Insurers are committed to standardizing electronic communications through Fast Healthcare Interoperability Resources (FHIR) frameworks, thereby improving efficiency. The plans include a commitment to reduce the number of services requiring prior authorization and ensure that existing authorizations remain valid during transitions between insurance plans. Additionally, they aim to foster better transparency and swift responses to authorization requests.
Despite prior attempts to reform preauthorization processes in recent years that failed to gain momentum, this new initiative has gained urgency, especially following heightened public unrest surrounding these issues. Dr. Mehmet Oz, CMS Administrator, remarked on the visible tensions surrounding healthcare access, referring to alarming incidents tied to dissatisfaction with coverage denials.
While cautioning about the unpredictability of implementing such reforms, Dr. Oz acknowledged that the federal government holds the potential to introduce mandatory regulations should the voluntary changes fail to materialize effectively. The pressing need for operational change reflects a broad acknowledgment within the industry that many existing preauthorization practices require reevaluation.
As stakeholders move towards digitizing and streamlining the preauthorization landscape, common procedures like cataract surgeries and routine deliveries remain overly subjected to cumbersome preauthorization requirements. These changes are essential for maintaining continuity in patient care while enhancing operational efficacy across healthcare systems in the U.S.
The Intersection of AI and Healthcare
In discussions about technological solutions, Congressman Gregory Murphy, a physician himself, remarked on the potential role AI can play in refining the preauthorization process. However, he cautioned against over-reliance on AI, emphasizing the importance of the quality and relevance of the data input into these systems. Misguided inputs could perpetuate existing denial patterns rather than alleviating them.
While proponents advocate for AI’s promise in improving preauthorization, critics remain concerned about its implementation in vital healthcare decisions. Insurers, including those cited in ongoing litigation, face scrutiny over the alleged inappropriate application of AI in their claims processing, raising fundamental questions about the intersection of technology and patient care.
