Data Privacy,
Data Security,
Healthcare
Voluntary Initiative Advocates for Standards and Patient Empowerment: A Privacy Perspective
The Trump administration has unveiled an initiative aimed at bolstering patient data interoperability across the healthcare sector. This initiative encourages technology companies, healthcare providers, and insurers to voluntarily adhere to specified standards and criteria for data sharing.
Named the “Make Health Technology Great Again” plan, the initiative, led by the U.S. Department of Health and Human Services and its Centers for Medicare and Medicaid Services (CMS), seeks to foster a collaborative environment where industry stakeholders can align with a framework for secure health information exchange.
Central to the plan is the promotion of voluntary compliance with a CMS Interoperability Framework, defined as an open and standards-based infrastructure. It also encourages the creation and utilization of third-party patient applications—such as conversational AI tools—to empower patients with personalized insights and facilitate better healthcare decisions.
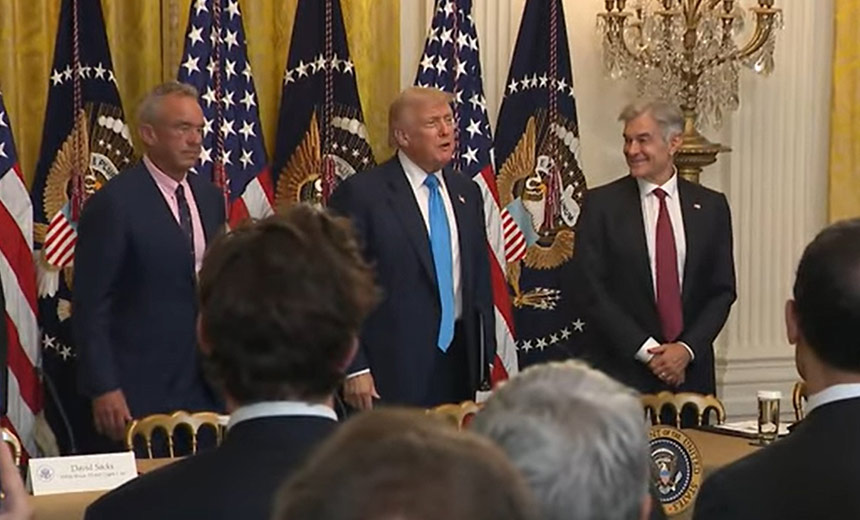
In announcing this initiative, President Trump asserted that it would allow patients to seamlessly transfer their medical records between providers, irrespective of the systems used. He emphasized that the plan would not involve the establishment of a centralized government database.
By engaging with industry participants, the CMS aims to evolve a more patient-centric ecosystem that reduces reliance on traditional methods, such as paper forms and fax machines, for exchanging health data. Currently, over 60 organizations, including major tech companies like Apple and Google along with health insurers and app developers, have pledged their support, with promises to deliver new capabilities by early 2026.
Patients will be empowered to retrieve their health records via networks aligned with CMS and personal health record applications, leveraging modern technologies like QR codes and smart health cards based on Fast Healthcare Interoperability Resources (FHIR) protocols.
However, despite the potential benefits, the initiative also raises privacy and security concerns. Experts caution that there may be risks associated with sharing health information through non-covered entities, especially if robust safeguards are not in place. The nuances of the plan’s privacy implications further complicate its overall acceptance in the healthcare community.
With this initiative resembling past attempts to establish secure nationwide health data exchanges, it is essential to note that efforts to enhance patient access to electronic health records span back over two decades, intersecting with multiple presidential administrations. The enduring complexity of patient data Access remains a critical challenge, despite advances in technology.
As the initiative unfolds, it will be instrumental for stakeholders to recognize the potential MITRE ATT&CK tactics at play, particularly regarding the frameworks for initial access, persistence, and privilege escalation. The consideration of such tactics may help guide the measures necessary to safeguard patient data while promoting interoperability.